Across the province, patients calling 911 encounter long wait-times for ambulances, with great consequences for their health and safety.
Municipal paramedic services across the province frequently face Code Blacks whereby there are no ambulances available to respond to 911 calls. Even outside of Code Blacks, services often have critically low ambulance availability.
In CUPE’s 2021 membership survey, 41% of CUPE EMS members said they experience Code Blacks daily. Another 24% said they experience them a few times a week.
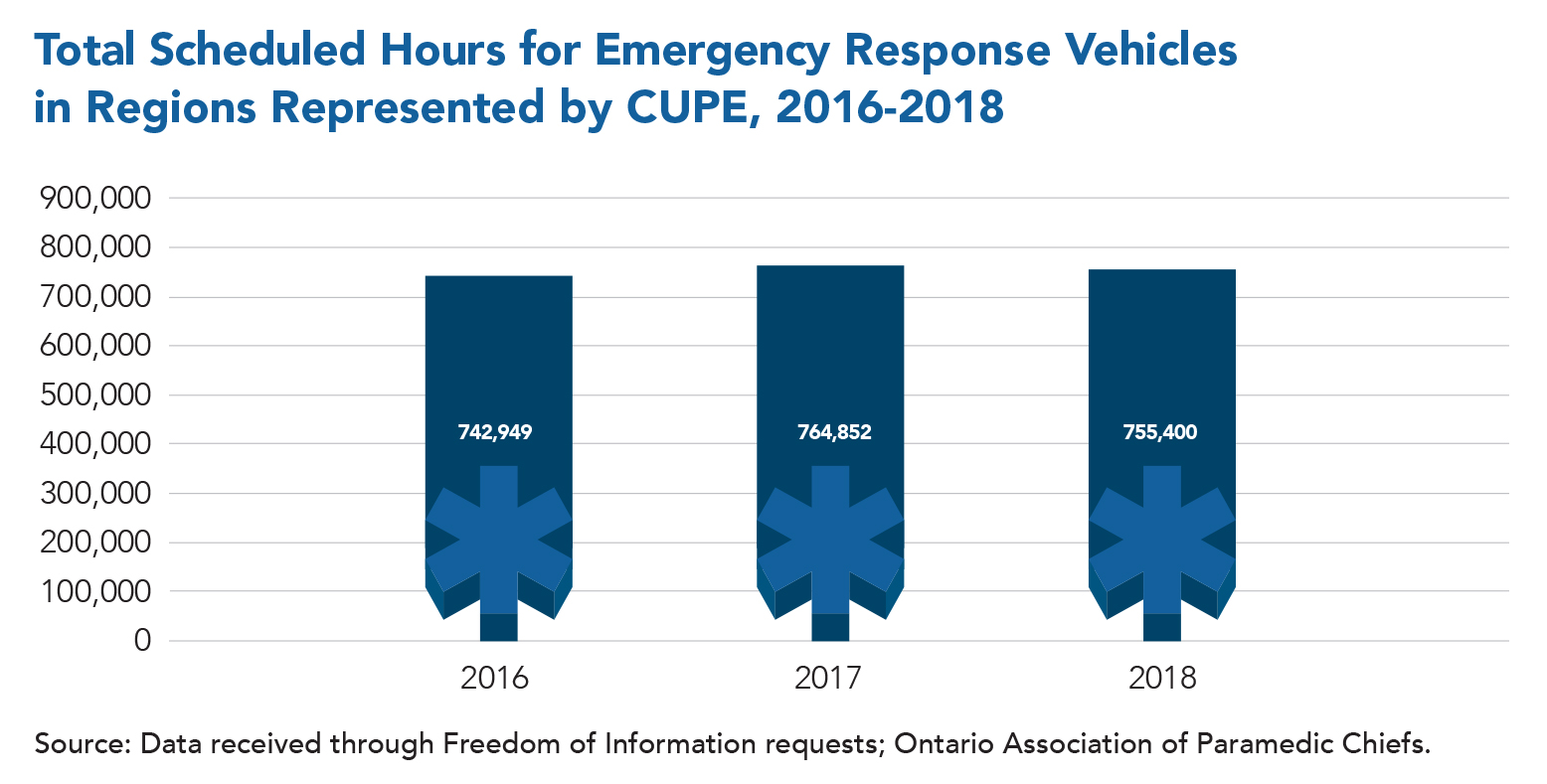
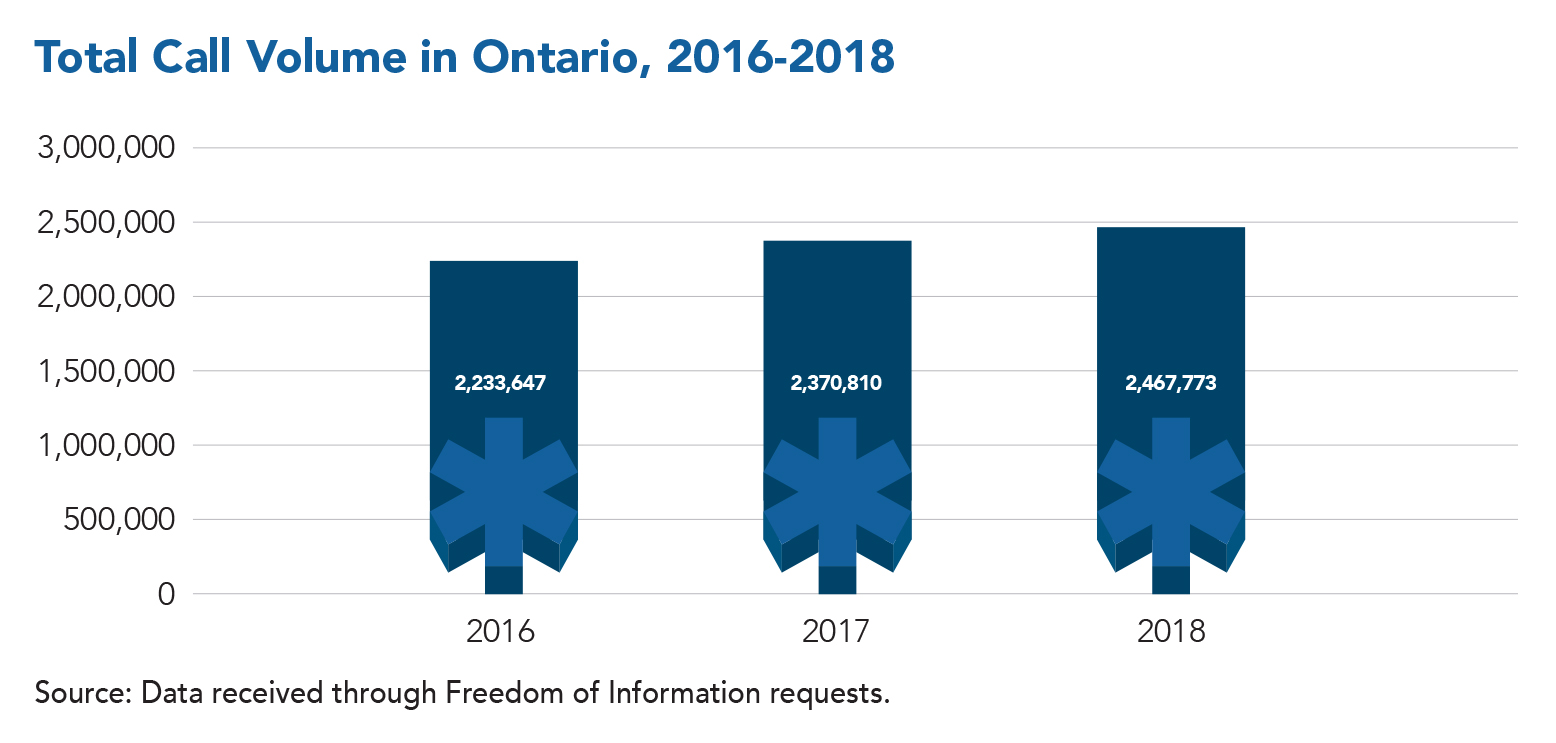
Based on Freedom of Information requests, CUPE found that while call volumes are increasing steadily, scheduled hours for ambulances are not keeping pace with demand. Ambulances are often taken off the road due to understaffing, as regional services are unable to recruit and retain enough paramedics.
The primary issue is underfunding by both the provincial and municipal governments, which have compromised care for patients who require emergency medical services.